RADICULOPATHY: WHAT IT IS AND HOW TO RECOVER FROM IT
Radiculopathy is a word that describes the injury to a nerve root related to compression in or around the spine. This condition is more commonly referred to as a pinched nerve. This nerve injury can cause a variety of symptoms including, but not limited to, pain, numbness, and weakness. In this post, we will explore the causes of this condition, how it should be evaluated, and how to treat it.
The Anatomy of Radiculopathy
Radiculopathy can occur at different levels of the spine and is, thus, typically broken down into cervical radiculopathy, thoracic radiculopathy, and lumbar radiculopathy.
Cervical Radiculopathy
The cervical spine is comprised of seven vertebral bodies, C1 through C7. Radiculopathy can occur in the cervical spine when one or multiple of the nerve roots is compressed. This issue more commonly occurs in the lower cervical nerve roots like C6 and C7.
Thoracic Radiculopathy
The thoracic spine is comprised of twelve vertebral bodies, T1 through T12. Radiculopathy can occur in the thoracic spine when one or multiple of the nerve roots in this region is compressed. Thoracic radiculopathy is much less common than the lumbar or cervical varieties, but it can still be a significant source of pain when it does occur.
Lumbar Radiculopathy
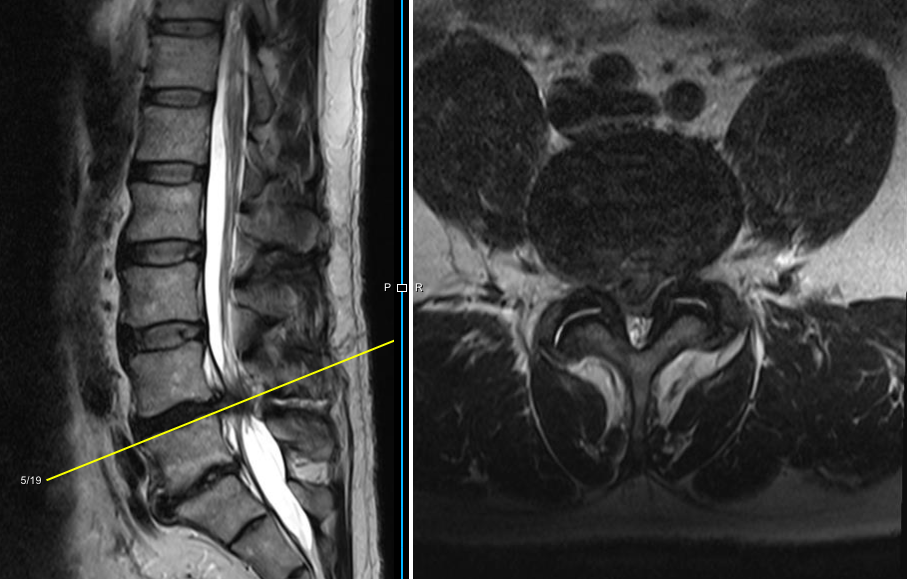
A large lumbar disc herniation causing spinal stenosis and symptoms of radiculopathy.
The lumbar spine is typically comprised of five vertebral bodies, L1 through L5. Radiculopathy can occur in the lumbar spine when one or multiple of the nerve roots in this region is compressed. The issue more commonly occurs in the lower lumbar spine at L5 or even S1, which is technically part of the sacral spine.
Signs and Symptoms of Radiculopathy
Radiculopathy is a condition that occurs when a spinal nerve root is compressed, irritated, or inflamed, leading to symptoms that radiate along the pathway of the affected nerve. The signs and symptoms of radiculopathy can vary depending on the location and level of nerve root involvement. The most characteristic symptom of radiculopathy is pain that follows the distribution of the affected nerve. The pain is often described as sharp, shooting, or burning and can travel from the spine to the specific areas supplied by the nerve. For example, in cervical radiculopathy, the pain may radiate down the arm, while in lumbar radiculopathy, it may travel down the leg. This type of pain from lumbar radiculopathy is often referred to as sciatica, or sciatic nerve pain. Patients with thoracic radiculopathy will usually complain of pain that radiates from the mid-back to the anterior chest wall on one side.
Individuals with radiculopathy may also experience sensations of numbness, tingling, or pins-and-needles in the areas supplied by the affected nerve, a sensory disturbance known as paresthesia. Radiculopathy can lead to muscle weakness in the muscles innervated by the affected nerve, and reflexes may become diminished or absent, depending on the level of involvement. Additionally, radiculopathy can cause altered sensations, such as heightened sensitivity to touch or decreased ability to discriminate temperature and texture.
In cases of cervical radiculopathy affecting the nerves that supply the hands and fingers, individuals may experience difficulties with fine motor skills, such as writing or buttoning shirts. Certain movements, such as bending, twisting, or coughing, may exacerbate radiculopathy symptoms and cause increased pain.
Radiculopathy vs. Myelopathy
Myelopathy and radiculopathy are both conditions that affect the nerves in the spine, but they differ in terms of the specific nerves involved and the areas of the nervous system affected.
Myelopathy is a condition that involves compression or injury to the spinal cord itself, which is the long, tube-like structure that runs through the spinal canal. The spinal cord is a crucial part of the central nervous system and carries nerve signals to and from the brain to the rest of the body. As a result, myelopathy can cause many of the same symptoms as radiculopathy but also can cause issues with balance and bowel/bladder incontinence.
Radiculopathy involves compression of the spinal nerves that emanate from the spinal cord, so the patient does not typically have the balance dysfunction that can be seen with myelopathy. Nerve root compression can lead to many of the other symptoms already described.
Distinguishing these two conditions is very important when evaluating patients with the cervical radiculopathy symptoms because myelopathy usually needs more urgent intervention to decompress the spinal cord.
Radiculopathy vs. sciatica
Sciatica is a term that describes back pain radiating down the leg past the knee. Therefore, lumbar radiculopathy is one condition that can cause sciatica, or sciatic nerve pain. Not all sciatica is caused by lumbar radiculopathy, but it is certainly one of the most common causes of sciatica.
Causes of Radiculopathy
Radiculopathy can be caused by various factors, with the most common cause being compression or irritation of the nerve roots as they exit the spinal cord.
Herniated Discs
One prevalent cause is a herniated disc, where the soft inner material of a disc pushes through its outer ring and presses against adjacent nerve roots. This issue is more common in younger patients, from 20 years old to 50 years old, and becomes less prevalent in the older population.
Spinal Stenosis
A radiculopathy patient with multilevel lumbosacral spondylolisthesis and secondary spinal stenosis.
Another common culprit is spinal stenosis, a condition characterized by the narrowing of the spinal canal or neural foramina, leading to pressure on the nerve roots. Degenerative disc disease and osteoarthritis can also contribute to radiculopathy, as they cause the breakdown of spinal structures and the formation of bone spurs that compress the nerves. Additionally, spondylolisthesis, a condition in which one vertebra slips forward over another, can cause nerve root compression, usually by creating spinal stenosis.
Other Causes
Other less frequent causes include spinal tumors, infections, and injuries that result in spinal fractures or dislocations. Understanding the underlying cause of radiculopathy is vital for developing an appropriate treatment plan to alleviate symptoms and prevent potential complications.
Risk Factors for Developing Radiculopathy
Several risk factors increase the likelihood of developing radiculopathy. One of the primary risk factors is age. As people age, the spinal structures tend to undergo degenerative changes, such as disc herniation and bone spurs, which can lead to nerve root compression and the development of radiculopathy. Additionally, occupations or activities that involve repetitive spine movements, heavy lifting, or prolonged sitting can increase the risk of lumbar radiculopathy, as they put additional stress on the spinal discs and structures, potentially leading to nerve compression over time. Obesity is also a significant risk factor, as excess body weight can contribute to increased pressure on the spine and accelerate degenerative changes. Genetics may play a role, as some individuals may have a genetic predisposition to developing conditions that contribute to radiculopathy, such as degenerative disc disease or spinal abnormalities. Finally, certain medical conditions like diabetes and autoimmune disorders can affect nerve health and increase the vulnerability to nerve compression and radiculopathy. Understanding these risk factors is crucial for identifying individuals who may be more prone to developing radiculopathy and implementing preventive measures or early intervention strategies.
Diagnosing Radiculopathy
In order to diagnose radiculopathy, a combination of medical history, physical exam, and diagnostic imaging. The healthcare provider will begin by discussing the patient's symptoms, including the location, duration, and characteristics of pain, numbness, or weakness. They will also inquire about any previous injuries, medical conditions, or activities that may be relevant to the diagnosis. A thorough physical examination is conducted to assess the patient's neurological function, muscle strength, reflexes, and sensory responses. The healthcare provider will check for any signs of nerve irritation or compression, as well as areas of tenderness along the spine.
Imaging Tests for Radiculopathy
Diagnostic imaging is crucial for confirming the diagnosis of radiculopathy and identifying the underlying cause. Commonly used imaging tests include Magnetic Resonance Imaging (MRI), Computed Tomography (CT) scan, and X-rays. Each test would be done in the specific area of the spine from where the symptoms might be emanating - cervical spine for neck and upper extremity, thoracic spine for mid-back and chest, and lumbar spine for low back and lower extremity.
MRI scans provide detailed images of the spinal structures, including the discs, nerve roots, and soft tissues. MRI is particularly useful for detecting herniated discs, spinal stenosis, and other structural abnormalities that can cause radiculopathy. CT scans can offer detailed cross-sectional images of the spine and may be used in conjunction with MRI for a more comprehensive evaluation of the bony structures. X-rays are primarily used to assess the alignment and stability of the spine and may be helpful in identifying fractures or degenerative changes. Nerves and nerve roots are not visible on X-ray, so it is a less useful imaging modality for evaluating radiculopathy.
Electromyography (EMG) and Nerve Conduction Studies (NCS)
In some cases, EMG/NCS may be performed to assess nerve function and identify specific areas of nerve root compression or damage. These tests are often useful in combination with detailed imaging studies to identify the exact area of nerve impingement as well as the degree of nerve injury and even prognosis for recovery.
Treating Radiculopathy
The treatment of radiculopathy aims to relieve pain, improve function, and enhance the individual's quality of life. The choice of treatment depends on the underlying cause of the radiculopathy, the severity of symptoms, and the patient's overall health. Conservative treatments are often the initial approach and may include relative rest, activity modification, chiropractic care, and acupuncture. Lifestyle modifications such as weight management and temporarily avoiding activities that exacerbate symptoms are also beneficial.
Physical Therapy and Medications
Physical therapy is a mainstay of radiculopathy treatment to improve posture, strengthen supportive muscles, and promote extremity flexibility. Sometimes, specific exercises like nerve glides can be useful in alleviating the symptoms. Medications can also be used to treat the symptoms of a pinched nerve. Nonsteroidal anti-inflammatory drugs (NSAIDs) can help manage pain and reduce inflammation while other medications like muscle relaxers and neuropathic pain medications can also help, especially in combination with a good physical therapy program.
Injection Care
An epidural steroid injection for lumbar radiculopathy.
If more aggressive treatment is needed, epidural steroid injections may be used to provide temporary relief by reducing inflammation around the compressed nerve root. These injections are typically done by a fellowship-trained physician with fluoroscopic, or x-ray, guidance. A cervical epidural steroid injection carries more risk than a lumbar injection, as there are important structures in and around the cervical spine that can be damaged with a misplaced injection.
Surgery
If conservative measures are not effective or if the radiculopathy is severe, surgical intervention may be considered. Surgical options vary based on the underlying cause and may involve procedures like discectomy (removal of herniated disc material), laminectomy (removing a portion of the lamina to relieve pressure on nerve roots), or spinal fusion (stabilizing the spine). The choice of surgery depends on factors such as the location of the affected nerve root and the extent of compression.
What Happens if Radiculopathy is Left Untreated?
If left untreated, radiculopathy can lead to a range of complications that can significantly impact an individual's quality of life. One of the primary concerns is the potential for developing chronic pain. Chronic pain not only affects physical well-being but can also have emotional and psychological consequences, leading to depression, anxiety, and decreased overall quality of life.
Additionally untreated radiculopathy can lead to worsening symptoms over time. The compression or irritation of nerve roots can progress, causing increased pain, numbness, and weakness in the affected areas. Prolonged nerve compression can also result in permanent nerve damage, which may result in long-term sensory and motor deficits that affect overall function.
How Long Does Radiculopathy Take to Heal?
The duration of healing for radiculopathy varies widely based on several factors, including the underlying cause, the severity of nerve compression, the individual's overall health, and the effectiveness of treatment. Mild cases of radiculopathy may resolve on their own or with conservative treatments within a few weeks to a few months. However, more severe cases or those involving chronic conditions may require longer healing periods, potentially extending to several months or even years.
Summary
Radiculopathy is a common condition that affects many people on a daily basis. There are multiple possible causes of radiculopathy that are usually determined by the age and comorbidities of the patient. Anyone dealing with radiculopathy symptoms, or a pinched nerve, should seek specialist care sooner rather later to confirm the diagnosis and develop an appropriate treatment plan.